Overview, pathophysiology and management
Introduction –
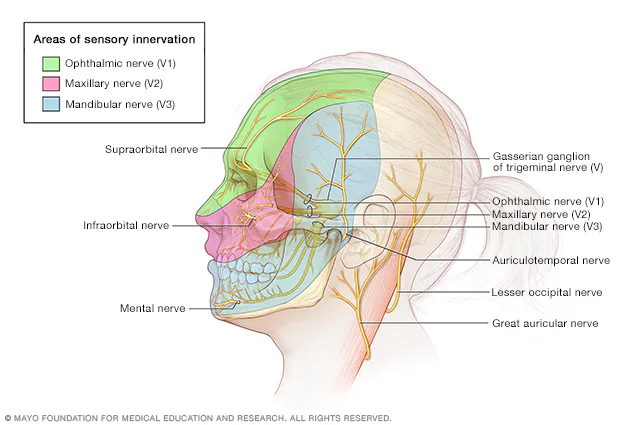
Trigeminal neuralgia (TN) is a long- lasting facial pain disorder that affects trigeminal cranial nerve v (nerve responsible for face sensation). It is characterized by sudden, severe and recurrent episodes of facial pain, often described as stabbing, electric shock- like, or burning in nature. TN can significantly impair quality of life, leading to emotional distress, anxiety and social withdrawal.
Epidemiology-
- It is more common in individuals over 50 years, with a slight female predominance.
- The annual incidence is estimated at 4–13 per 100,000 people worldwide.
- Most cases are unilateral, affecting one side of the face, commonly in the maxillary (V2) and mandibular (V3) divisions.
- Bilateral involvement is rare and may indicate secondary causes, such as multiple sclerosis.
Etiology and Pathophysiology
The exact mechanism of TN is not fully understood, but two main types are recognized:
1. Classical Trigeminal Neuralgia
It caused by vascular compression of the trigeminal nerve at the root entry zone near the brainstem.
Compression by arteries (commonly the superior cerebellar artery) leads to Demyelination and Hyperexcitability of nerve fibers.
2. Secondary (Symptomatic) Trigeminal Neuralgia
-Caused by underlying conditions such as:
- Multiple sclerosis
- Tumors compressing the trigeminal nerve
- Arteriovenous malformations
- Trauma or infection
Pathophysiology-
Demyelination or nerve injury leads to aberrant electrical signaling, causing paroxysms of intense pain.
Even mild stimuli, like touch, speaking, or chewing, can spark attacks due to hyperactive nerve signaling.
Clinical Features
- Pain Character: Sudden, unilateral, sharp, electric shock-like, burning, or stabbing.
- Duration: Each episode lasts seconds to a few minutes but may recur multiple times daily.
- Triggers: Light touch on the face, chewing, talking, brushing teeth, or wind.
- Distribution: Follows the trigeminal nerve branches:
Ophthalmic (V1)
Maxillary (V2)
Mandibular (V3)
Red flag symptoms: Bilateral pain, sensory loss, or weakness may indicate secondary causes.
Diagnosis
Diagnosis of TN is primarily clinical, based on history and symptoms Investigations include:
- Magnetic Resonance Imaging (MRI): To detect vascular compression or secondary causes.
- MRI with MR angiography (MRA): Helps visualize vascular loops compressing the nerve.
- Neurological examination: Usually normal between attacks.
- Pain diaries: To document triggers and frequency.
Management
- Medical Management
- Anticonvulsants, like carbamazepine
- Antidepressants, like Amitriptyline
- Muscle relaxant, like baclofen.
2. Surgical Interventions
Considered when medical therapy is inadequate or poorly tolerated:
Microvascular Decompression (MVD): Relieves vascular compression; high success rate for classical TN.
Gamma Knife Radiosurgery: Non-invasive option using focused radiation to disrupt nerve signaling.
Percutaneous Techniques: Balloon compression, glycerol rhizotomy, or radiofrequency ablation.
Physiotherapy management–
Physiotherapy promotes, maintains, and restores the physical, psychological, and social wellbeing of an individual by the use of different techniques. The physiotherapy treatment of TN focusses on the patient’s goals and needs.
According to Reeta et.al in their study done in 2016, the physiotherapy treatment of TN patients is efficient and includes:
- Electrical Stimulation (TENS) as the most effective and most often used technique
- Interferential Therapy (IFT)
- Ultrasound
Physiotherapy Management will also aim at reducing pain and improve the ability to carry on with the activities of daily living (ADLs) by using..
- Acupuncture to relieve facial pain and pressure
- Isometric neck exercises
- Relaxation techniques such as deep breathing exercises
- Cardiovascular exercises to improve health and fitness levels
- Functional Activities for problems associated with ADLs
- Patient’s education on diet, management of sleep, and rest
- Advice on how to avoid using cold water for drinking and washing their face but also chewing with the non affected side.
Physiotherapy can alternatively play different roles in the management of TN in educating, advising, and motivating patients. Although physiotherapy treatment is effective in the Management of TN, there is a need for awareness of its role among the general public.
3. Lifestyle and Supportive Measures
Avoid triggers (extreme cold, facial touch) during attacks. Psychological support may assist chronic pain-related anxiety or depression.
Prognosis-
- TN is chronic and progressive, but treatment can significantly relief pain and improve quality of life.
- Recurrence after initial treatment is common, particularly with medical therapy alone.
- Early diagnosis and intervention are key to preventing long-term nerve damage and complications.
Recent Advances
- Neuromodulation techniques such as trigeminal nerve stimulation are emerging.
- Genetic studies are exploring predisposition and molecular mechanisms of nerve hyperexcitability.
- Imaging innovations improve detection of microvascular compression, optimizing surgical planning.
Conclusion
Trigeminal neuralgia is a debilitating condition that demands timely diagnosis and multimodal management. Advances in imaging, pharmacotherapy, and minimally invasive surgery have improved outcomes, but continued research is necessary to fully understand the pathophysiology and provide long-term relief for patients.
References –
- Gambeta E, Chichorro JG, Zamponi GW. Trigeminal neuralgia: An overview from pathophysiology to pharmacological treatments. Mol Pain. 2020 Jan-Dec;16:1744806920901890. [PMC free article] [PubMed]
- Maarbjerg S, et al. Trigeminal Neuralgia – Diagnosis and Treatment. Cephalalgia. 2017;37(7):648–657.
- Cruccu G, et al. EFNS Guidelines on Trigeminal Neuralgia. Eur J Neurol. 2008;15:1013–1028.
- Zakrzewska JM. Trigeminal Neuralgia. BMJ. 2013;347:f7336.
- Headache Classification Committee of the International Headache Society. ICHD-3. Cephalalgia. 2018;38(1):1–211.
- Bašić Kes V, Zadro Matovina L. Accommodation to Diagnosis of Trigeminal Neuralgia. Acta Clin Croat. 2017 Mar;56(1):157-161. [PubMed]
- Truini A, Prosperini L, Calistri V, Fiorelli M, Pozzilli C, Millefiorini E, Frontoni M, Cortese A, Caramia F, Cruccu G. A dual concurrent mechanism explains trigeminal neuralgia in patients with multiple sclerosis. Neurology. 2016 May 31;86(22):2094-9. [PubMed]