A Comprehensive Overview
Introduction
Schizophrenia is a Chronic and Severe Mental Disorder that affects how a person thinks, feels and behaves. It is characterized by distortion in Perception, Impaired Reality Testing, disorganized thinking and Difficulties in Social and Occupational Functioning.
Globally about 24 million people (1 in 300 adults) live with Schizophrenia, making it a significant Public Health Concern (WHO, 2024).
Historical Background
The term Schizophrenia was first Introduced by Swiss Psychiatrist Eugen Bleuler in 1908, derived from the Greek words schizo (split) and phren (mind), to describe the fragmentation of thought processes and Emotional Responsiveness. Earlier, Emil Kraepelin referred to it as “Dementia Praecox.”
What is schizophrenia?
Schizophrenia is a Mental Health condition that affects how you think, feel , and behave. It can make it hard to know what is real and what is not.
It can lead to symptoms like ..
DELUSION, HALLUCINATION AND PSYCHOSIS.
While it’s a life long disorder, treatment can help you manage symptoms so you can feel better.
Etiology and Risk Factor
The exact cause of Schizophrenia is unknown, but it is considered Multifactorial, Involving:
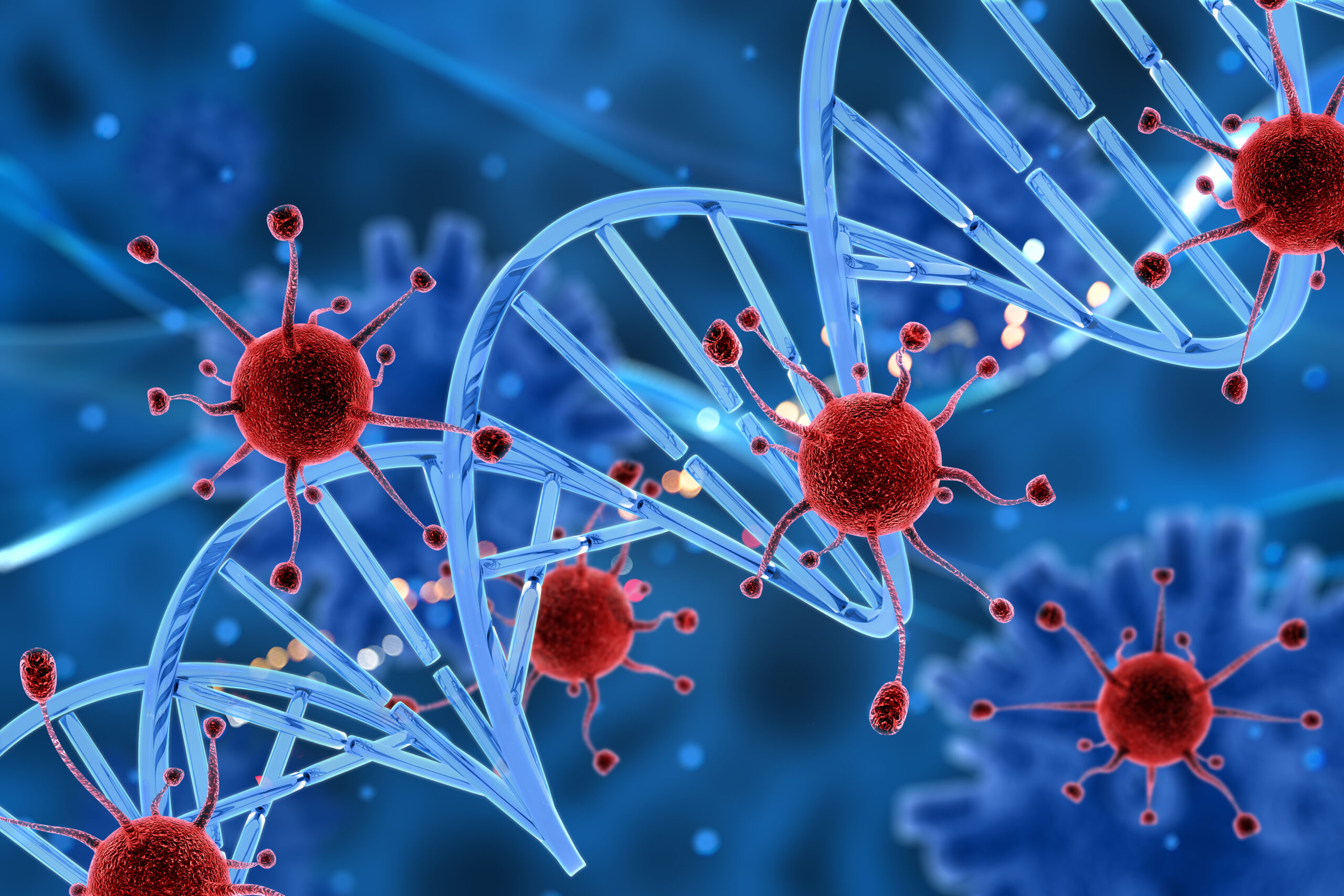
1. Genetic Factors – First-degree relatives of Patients have a 10% risk compared to 1% in the General population.
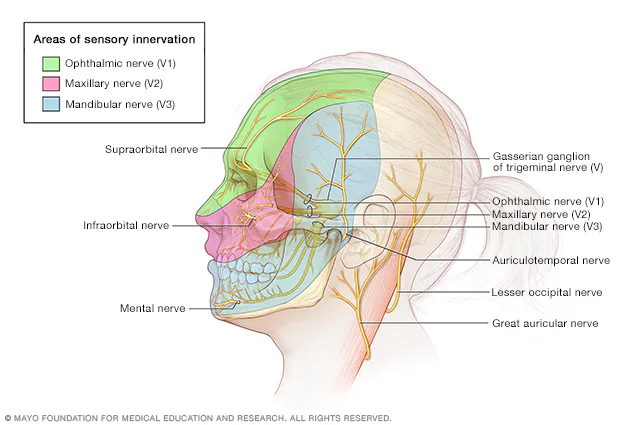
2. Neurobiological Changes – Dopamine Dysregulation, Glutamate Abnormalities, and Altered Brain Structures (Enlarged Ventricles, Reduced Gray Matter).
3. Environmental Factors – Prenatal Infections, Obstetric Complications, Childhood Trauma, Urban Upbringing.
4. Psychosocial Stressors – Social Isolation, Poverty, and Family Conflicts can Precipitate Episodes in Vulnerable Individuals.
Clinical Feature
Symptoms are categorized into three major groups:
Positive Symptoms (excess of normal functions):
- Delusions (False Beliefs, e.g. Persecution, Grandeur)
- Hallucinations (Commonly Auditory)
- Disorganized Speech and Behavior
Negative Symptoms (Loss of Normal Functions):
- Affective Fattening
- Alogia (Poverty of Speech)
- Anhedonia (Inability to feel pleasure)
- Avolition (Lack of Motivation)
Cognitive Symptom
- Impaired Attention and Working Memory.
- Poor Executive Functioning
- Difficulty in Decision-Making
Diagnosis
Diagnosis is primarily clinical, based on DSM-5 (APA, 2013) or ICD-11 (WHO, 2022) criteria.
Key features for DSM-5:
Two or more symptoms (Delusions, Hallucinations, Disorganized speech, Disorganized Behavior, Negative Symptoms) lasting ≥ 6 months, with at least 1 month of Active-Phase symptoms.
Investigations like MRI, CT, or EEG may be done to rule out Organic causes but are not diagnostic.
Treatment and Management
Treatment follows a Biopsychosocial Approach:
1. Pharmacological interventions
Antipsychotics (first-line):
- Typical: Haloperidol, Chlorpromazine
- Atypical: Risperidone, Olanzapine, Clozapine (for Treatment-Resistant Cases)
Long-acting injectable improve compliance.
2. Psychosocial interventions
Cognitive Behavioral Therapy (CBT)
Family Psychoeducation
Social Skills Training and Vocational Rehabilitation.
Lifestyle Support in Schizophrenia
While Medication is the Cornerstone treatment of Schizophrenia, Lifestyle Modifications and Supportive Strategies play a crucial role in improving quality of life, reducing relapses, and enhancing overall functioning.
1. Healthy Routine and Structure
Maintaining a regular sleep–wake cycle stabilize mood and reduce Hallucinations or Disorganized thoughts.
A daily routine (proper meals, exercise, rest, and activities) can reduce stress and confusion.
2. Balanced Nutrition
Diets rich in Omega-3 Fatty Acids, whole grains, Fruits, and Vegetables support Brain Health. Limiting sugar, Processed Foods, Caffeine, and Alcohol can reduce symptom Exacerbation.
Deficiency in vitamins (especially Vitamin D and B12) should be monitored and corrected.
3. Physical Activity
Regular Aerobic Exercise refine Cognition, Reduces Negative symptoms, and amend social engagement.
WHO recommends 150 minutes of Moderate Physical Activity per week.
4. Stress Management
Stress can trigger Psychotic relapses. Practices Yoga, Meditation, Mindfulness, and Relaxation Techniques help in coping.
5. Sleep Hygiene
Maintaining consistent bedtime routines, Avoiding late-night screen exposure and caffeine, Using relaxation rituals (reading, light stretching, calming music).
6. Social and Family Support
Strong family involvement in treatment improves medication adherence and relapse prevention.
Peer support groups reduce stigma and feelings of isolation.
Engaging in Community Programs Enhance Social Functioning and Vocational skills.
7. Avoidance of Substance Use
Alcohol, Nicotine, and Recreational drugs worsen Psychosis and interfere with Antipsychotic Medication.
8. Adherence to Treatment
Using Pill organizers, reminders, or long-Acting Injectable Antipsychotics helps in Maintaining consistent medication use, Regular follow-ups with Psychiatrists are essential.
9. Occupational and Vocational Rehabilitation
Supported Employment Programs and Skill-Training Workshops help patients regain independence, Meaningful work improves self-esteem and reduces negative symptoms.
Prognosis-
Approximately 20% of patients Achieve Good Recovery,
50% have Intermittent Relapses, and 30% Experience Chronic Disability.
Early Diagnosis, Medication Adherence, Strong Family Support, and Reduced Substance Abuse Improve Outcomes.
Recent Advances-
- Digital Psychiatry: Smartphone apps for Monitoring symptoms.
- Neuroimaging Biomarkers: Research on Early Detection.
- Novel Drugs: Targeting Glutamate and Inflammatory Pathways.
- rTMS (Repetitive Transcranial Magnetic Stimulation): Investigated for treatment-Resistant Hallucinations.
Conclusion-
Schizophrenia is a Debilitating yet Treatable disorder. With Early Intervention, Personalized Treatment, Family support, and Community integration, Patients can lead meaningful and productive lives. Ongoing Research into Genetics, Brain Imaging, and Novel Therapeutics holds promise for better outcomes in the future.
References-
- World Health Organization (2024). Schizophrenia Fact Sheet.
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5).
- Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s Synopsis of Psychiatry. 12th ed. Wolters Kluwer; 2022.
- Frese FJ, 3rd, Knight EL, Saks E. Recovery from schizophrenia: with views of psychiatrists, psychologists, and others diagnosed with this disorder. Schizophr Bull. 2009 Mar;35(2):370–80. doi: 10.1093/schbul/sbn175. PMID: 19304812. [PMC free article] [PubMed] [CrossRef]
- Buchy L, Cadenhead KS, Cannon TD, et al. Substance use in individuals at clinical high risk of psychosis. Psychol Med. 2015;45(11):2275–84. PMID: 25727300. [PMC free article] [PubMed]
- Goerke D, Kumra S. Substance abuse and psychosis. Psychiatr Clin North Am. 2013;22(4):643–54. PMID: 24012078. [PubMed]
- Mesholam-Gately RI, Gibson LE, Seidman LJ, et al. Schizophrenia and co-occurring substance use disorder: reward, olfaction and clozapine. Schizophr Res. 2014;155(1–3):45–51. PMID: 24685823. [PubMed]
- De Witte NA, Crunelle CL, Sabbe B, et al. Treatment for outpatients with comorbid schizophrenia and substance use disorders: a review. Eur Addict Res. 2014;20(3):105–14. doi: 10.1159/000355267. PMID: 24192558. [PubMed] [CrossRef]