An Overview-
Introduction –
Attention Deficit Hyperactivity Disorder (ADHD) is one of the most Prevalent Neurodevelopmental Disorders, it is recognized as a Chronic Disorder of Executive Functioning rather than a Transient Childhood Problem.
ADHD was first described in the Early 20th century as “Minimal Brain Dysfunction.”
The DSM-5 (2013) and ICD-11 (2019) define ADHD as a pattern of persistent symptoms of inattention and/or Hyperactivity-impulsivity that interfere with normal development.
Global prevalence: 5–7% in school-aged children (Polanczyk et al., 2015).
Indian prevalence: 1.6% to 17.9% across states (Indian Journal of Psychiatry, 2022).
Higher rates in boys (3:1 ratio), though inattentive subtype is more common in girls.
What Is ADHD?
ADHD ( Attention- Deficit/ Hyperactivity Disorder) is a condition that affects how your Brain works. Despite its name, ADHD doesn’t mean that you lack Attention. It means that it’s harder for you to control your attention or direct it to certain tasks. AFHD causes symptoms like difficulty focusing, trouble sitting still and Impulsive Behaviors. But it also you to “Get in the Zone” Hyperfocus on things you really enjoy.
Etiology and Risk Factor-
The exact cause of ADHD Remains Multifactorial. Research suggests the following contributing factors:
- Genetic Influences – Heritability Estimates Range from 70–80%.
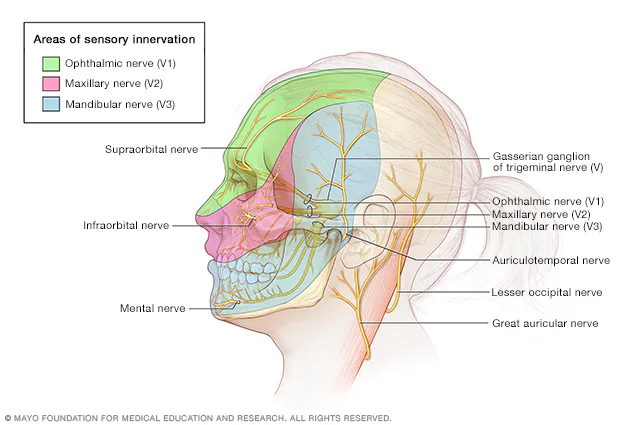
- Neurobiological Factors – Dysfunctions in Dopaminergic and Noradrenergic Pathways; Altered Activity in the Prefrontal Cortex and Basal Ganglia.
- Environmental Influences – Prenatal Exposure to Alcohol, Nicotine, or Maternal Distress, Low Birth Weight, lead Exposure.
- Psychosocial Factors – Family stress, Poor parenting styles, and Chaotic Environments can Exacerbate Symptoms, though they are not Direct Causes.
Clinical Features-
Symptoms typically present before the age of 12 and manifest in different settings (school, work, home). According to the DSM-5, ADHD is categorized into three presentations:
- Predominantly Inattentive Type
- Difficulty sustaining attention
- Careless mistakes in tasks
- Easily distracted or forgetful
- Predominantly Hyperactive-Impulsive Type
- Excessive fidgeting or restlessness
- Difficulty remaining seated
- Interrupting or intruding in conversations
- Combined Type
- A mix of both Inattentive and Hyperactive-Impulsive symptoms.
Impact-
ADHD significantly affects quality of life:
- Academic and occupational – Poor performance, unfinished tasks, frequent job changes.
- Social – Strained relationships, poor peer interaction, risk-taking behaviors.
- Psychiatric comorbidities – Depression, anxiety disorders, conduct disorder, and substance use are common.
Diagnosis-
Diagnosis requires:
- Comprehensive clinical evaluation
- DSM-5 criteria (symptoms persisting for at least 6 months, present in two or more settings, and causing impairment).
- Use of rating scales such as the Conners’ Rating Scale or ADHD Rating Scale (ADHD-RS).
Differential diagnoses include Learning Disabilities, Anxiety disorders, and Mood Disorders.
Management-
Management of ADHD is multimodal, combining pharmacological and non-pharmacological approaches:
1. Pharmacological Treatment
- Stimulants: Methylphenidate, Amphetamines – first-line treatment.
- Non-stimulants: Atomoxetine, Guanfacine, Clonidine – for patients intolerant to stimulants.
2. Behavioral Interventions
- Parent training in behavior management
- Classroom modifications (structured tasks, regular breaks)
- Cognitive-behavioral therapy (CBT)
3. Lifestyle Modifications
- Physical Activity – Regular exercise (30- 45 mint/ day). Activity like Yoga, Material Art, Team support Improve self Discipline and Social functioning.
- Sleep Hygiene – These patients commonly suffer from delayed sleep phase syndrome.
Recommendation – Fixed bedtime/ waking -up Routine, Limiting caffeine and late night screen time.
- Digital use Management –
American Academy of Pediatrics Recommend – < 2 hours / day screen time for children, Promoting Screen free Meals and Bedtime.
- Stress Reduction and Mindfulness – Breathing Exercise & Meditation lower hyperactivity.
- Structure Routine – Consistent Schedule for Meals, Homework, play time Reduce Distractibility.
Recent Trends in Research-
- Neuroimaging studies Highlight reduced Cortical Thickness in children with ADHD.
- Digital therapeutics (computerized cognitive Training, mobile apps) are being explored.
- Genomic research has Identified candidate genes (e.g., DRD4, DAT1) linked to ADHD susceptibility.
- Indian context: Studies indicate ADHD prevalence in Indian children ranges between 1.6% and 17.9%, with rising recognition in urban and rural populations.
Conclusion-
ADHD is a chronic yet manageable condition. Early diagnosis, tailored treatment, and strong family-school collaboration are crucial for improving outcomes. With ongoing research in genetics, neurobiology, and digital health, future strategies promise more personalized and effective interventions.
References-
- Faraone SV, Biederman J, Mick E. The age-dependent decline of ADHD: a meta-analysis of follow-up studies. Psychological Medicine. 2006.
- World Health Organization. International Classification of Diseases (ICD-11). 2019.
- Indian Journal of Psychiatry (2022): Prevalence and clinical profile of ADHD in Indian children.
- Biederman, J., Mick, E., Faraone, S.V., Braaten, E. et al.(2002) ‘Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic’, The American Journal of Psychiatry, 159(1), pp. 36–42.
- Bonvicini, C., Faraone, S.V. and Scassellati, C. (2016) ‘Attention-deficit hyperactivity disorder in adults: a systematic review and meta-analysis of genetic, pharmacogenetic and biochemical studies’, Molecular Psychiatry, 21(7), p. 872–84.
- Bradley, C. (1937) ‘The behavior of children receiving benzedrine’, The American Journal of Psychiatry, 94, pp. 577–585.
- Cantwell, D.P. (1975) ‘Genetics of hyperactivity’, The Journal of Child Psychology and Psychiatry, 16, pp. 261–264.