Introduction
Alzheimer’s disease (AD) is a progressive Neurodegenerative disorder and the most
common cause of Dementia worldwide. It gradually destroys memory, thinking skills, and
the ability to carry out daily activities. According to the World Health Organization (WHO,
2024), more than 55 million people are living with dementia, and Alzheimer’s contributes
to 60–70% of these cases.
What Happens in the Brain?
In Alzheimer’s disease, abnormal protein deposits disrupt normal brain function:
- Amyloid plaques (clumps of beta-amyloid protein) build up between nerve cells.
- Tau tangles (twisted fibers inside neurons) block nutrient transport.
- Neurons lose connections and die, leading to brain shrinkage, especially in
memory-related areas like the hippocampus.
Causes and Risk Factors
The exact cause remains unclear, but multiple factors contribute:
- Age – Risk increases significantly with age.
- Genetics – Mutations in genes associated with inherited from. 70% risk is linked to
genetics. - Family history – Having a close relative with AD raises chances.
- Lifestyle factors – Obesity, Diabetes, Smoking, High blood pressure, and Sedentary
lifestyle. - Brain health – Traumatic brain injury and low mental stimulation may contribute.
Symptoms
Alzheimer’s symptoms worsen over time, typically progressing through stages:
- Early stage: Mild forgetfulness, trouble finding words, misplacing items.
- Middle stage: Increasing memory loss, confusion, difficulty in daily tasks (like
bathing or dressing), emotional outburst. - Late stage: Severe memory decline, loss of communication ability, complete
dependence on caregiver.
Diagnosis
- Medical history ( comprehensive assessment ) including cognitive and Memory test
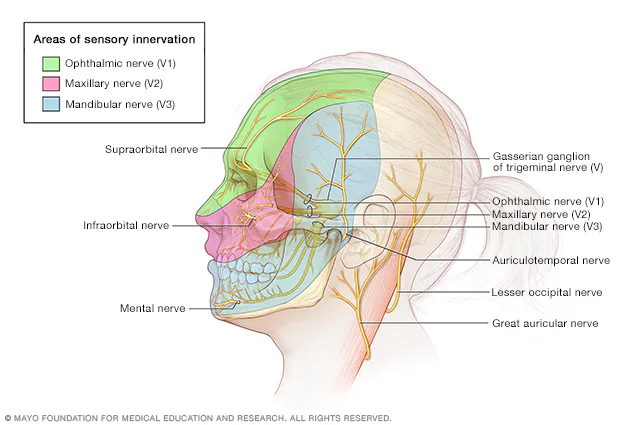
(MMSE). - Neurological exams (balance, senses & reflexes) Brain imaging (MRI, PET scans).
- Biomarkers – measuring amyloid and tau proteins in cerebrospinal fluid (CSF).
Treatment and Management
Currently, there is no cure for Alzheimer’s disease, but treatments help slow progression
and manage symptoms:
Medications
- Cholinesterase inhibitors (Donepezil, Rivastigmine, Galantamine) – improve
memory, judgment problem and cognition. - NMDA receptor antagonist (Memantine) – reduces symptoms in moderate-to-severe
AD. - New therapies – Lecanemab (FDA approved 2023) targets amyloid plaques.
Lifestyle Modification-
Regular physical activity ( aerobic exercise).
- Brain-stimulating activities (reading, puzzles)
- Healthy diet (Mediterranean/DASH diet)
- Social engagement.
- Supportive Care.
- Counseling for patients and families.
- Creating a safe, familiar living environment.
- Caregiver support to reduce burnout.
Prevention Strategies
Although Alzheimer’s cannot always be prevented, certain measures may lower risk:
- Controlling blood pressure, cholesterol, and diabetes
- Regular exercise
- Balanced diet rich in fruits, vegetables, whole grains, omega-3
- Avoiding smoking and excessive alcohol
- Staying mentally and socially active
Conclusion
Alzheimer’s disease is not only a medical challenge but also a social and economic
burden. With aging populations worldwide, the number of cases is expected to triple by 2050 offer hope for better management. Raising awareness, supporting caregivers, and investing
in research remain crucial steps in fighting this devastating disease.
References-
- Zhao QF, Tan L, Wang HF, et al. The prevalence of neuropsychiatric symptoms in
Alzheimer’s disease: Systematic review and meta-analysis. J Affect Disord. 2016 Jan
15;190:264–71. doi: 10.1016/j.jad.2015.09.069. PMID: 26540080. [PubMed]
[CrossRef] - Alzheimer’s Association. What is Alzheimer’s?; 2018. www.alz.org/alzheimers
dementia/what-is-alzheimers. Accessed on November 2 2018. - Centers for Disease Control and Prevention. Alzheimer’s Disease. 2018. www
.cdc.gov/aging/aginginfo/alzheimers.htm. Accessed on November 2 2018. - Harrison’s Principles of Internal Medicine, 21st Edition.
- Guyton and Hall, Textbook of Medical Physiology, 14th Edition.
- Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter: diagnosis of
dementia (an evidence-based review). Report of the Quality Standards
Subcommittee of the American Academy of Neurology. Neurology. 2001 May
8;56(9):1143–53. PMID: 11342678. [PubMed] - Shaw LM, Arias J, Blennow K, et al. Appropriate use criteria for lumbar puncture and
cerebrospinal fluid testing in the diagnosis of Alzheimer’s disease. Alzheimer’s &
dementia : the journal of the Alzheimer’s Association. 2018 Nov;14(11):1505–21.
doi: 10.1016/j.jalz.2018.07.220. PMID: 30316776. [PMC free article] [PubMed]
[CrossRef]