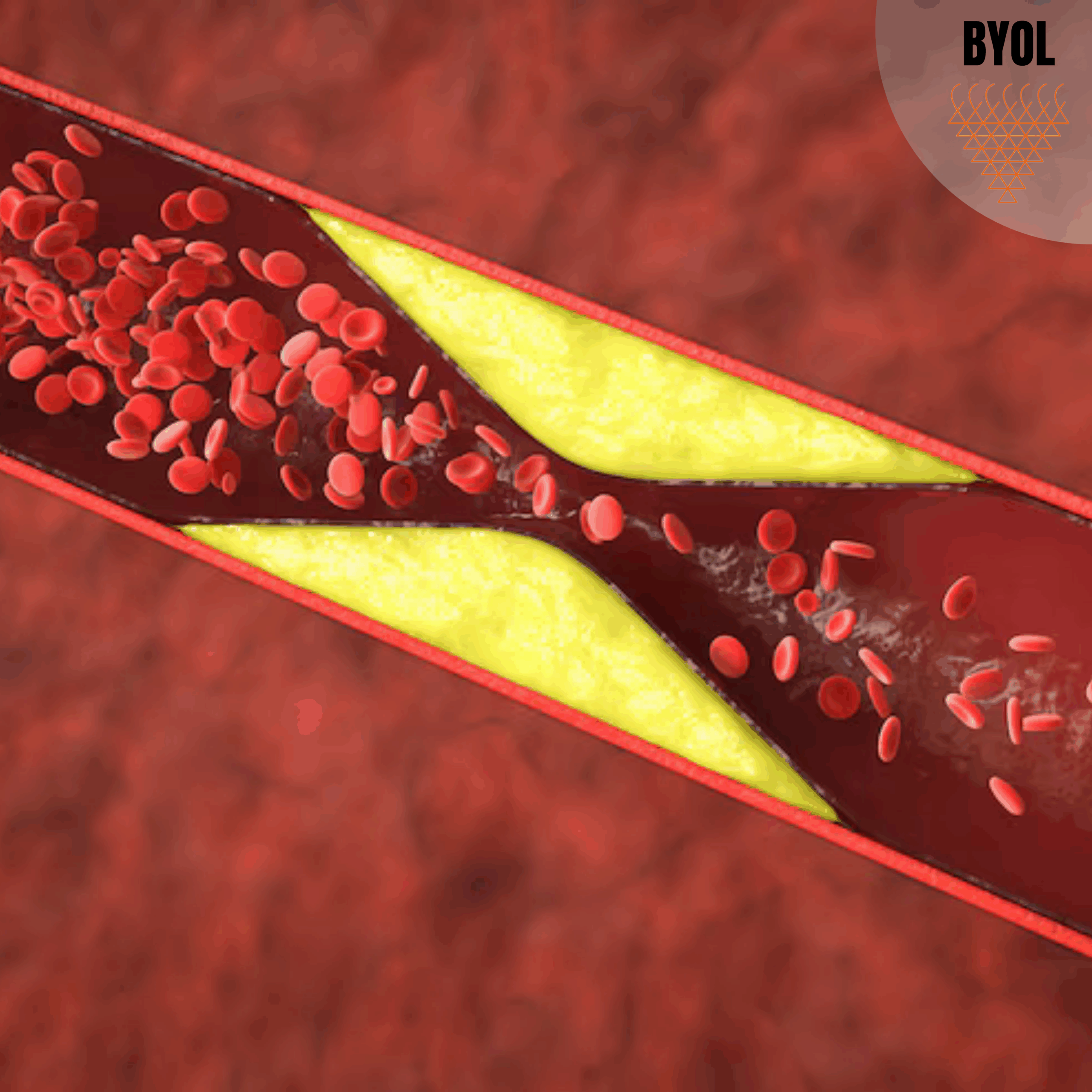
Atherosclerosis is a non-communicable disease (NCD) characterized by the stiffening of arterial walls due to the formation of atherosclerotic plaques, and being a multifactorial NCD, it has been a leading and chief cause of mortality across the globe. Cardiovascular diseases (CVDs) are causing an economic burden in all nations, with an additional greater impact in low- and middle-income nations. So far, the majority of efforts aimed at lowering the burden of atherosclerosis have been directed towards the control of various modifiable risk factors. Despite significant efforts towards the alleviation of the burden of CVDs, the evident morbidity, mortality, and loss of resources continue to persist, which leads researchers to look for novel ways to overcome it.
Innate as well as adaptive immunity are implicated in the pathogenesis of atherosclerosis, which is precipitated by lipid deposition and inflammatory mechanisms. Vaccination, as a major prevention strategy to induce a targeted immune response to antigens, has been applied for some bacterial and viral illnesses for decades. In recent years, vaccines for NCDs like cancer, atherosclerosis, hypertension, Alzheimer’s disease, and diabetes have been developed and also successfully used in certain autoimmune diseases. Nevertheless, regarding atherosclerosis, this approach is not as straightforward and uncomplicated as it appears at first glance. Vaccination may be an attractive option, and, likely, a promising and intriguing way to lighten the burden of the disease. A 1996 study by Ameli and his colleagues demonstrated that immunization with LDL and OxLDL decreased atherosclerotic lesions in the proximal aorta of rabbits by 74% and 48%, respectively. Despite considerable efforts in this area, vaccination against atherosclerosis remains in its early stages.
Role of the Immune System in Atherosclerosis
Innate immune system
Innate immune response is the primary defense of the host against the pathogen and is characterized by rapid and unsophisticated responses. It comprises immune cells like neutrophils, mast cells, macrophages, and natural killer (NK) cells.
- Neutrophils have been found to be involved in the subsequent phase of atherosclerosis and have been discovered in ruptured atherosclerotic plaques.
- Mast cells are triggered at the sites of plaque rupture and are exocytosed and degranulated, leading to destabilization of the atherosclerotic plaque.
- NK cells have been found to be involved in the early stage of atherosclerosis, but the role of these immune cells in the atherosclerosis process has not been clearly understood.
- Macrophages are the predominant inflammatory cells of the innate immune system that participate in atherosclerosis development and transmit immune signals to the adaptive immune system.
Adaptive immune system
- Adaptive immune cells have been shown to play an essential function in the atherosclerosis process, where nonfunctional adaptive immune cells in mice have lead to reduced lesion development.
- Unlike the innate immune system, the adaptive immune system is characterized by a delayed response and has a high specificity towards its target. Various types of immune cells are engaged in the adaptive immune system, including dendritic cells (DCs), T cells, B cells, and macrophages.
- The majority of T cells found in the atherosclerotic lesions are CD3+, CD4+, and TCR αβ+. When T cells identify a distinct antigen presented by an antigen-presenting cell (APC), it triggers an adaptive immune response towards that particular antigen.
- Some T cells within the atherosclerotic lesion might have a key role in producing interleukin 17 (IL-17), which is used in the process of vaccination. Among T cell population, T helper (Th)1, Th2, Th17, and regulatory T cells (Tregs) are significant and are vaccine-related.
- It has been shown that Th1 cells predominantly occur in atherosclerotic lesions and induce atherosclerosis through INF-ϒ production and TNF-α. INF-ϒ induces macrophage and endothelial cell activation, which leads to more secretion of adhesion molecules, proinflammatory cytokines, and chemokines, and consequently results in more recruitment of T cells. INF-ϒ supports the production of proteases and inhibits the production of collagen, which results in plaque instability.
- IL-3, IL-4, IL-5, IL-9, IL-10, and IL-13, are the so-called “anti-atherosclerotic cytokines” produced by Th2 cells, which possess inhibitory activities on Th1 cells, thus playing an anti-inflammatory role.
- It has been demonstrated that oral administration of atherosclerosis-associated antigens like heat shock protein 60 (HSP60) and oxidized low-density lipoprotein (OxLDL) enhances the population of Foxp3-expressing Tregs in various organs, which results in reduced formation of atherosclerotic lesions.
- B cells, a key subset of immune cells, play a critical role in antibody production against a particular antigen. B1 cells have been demonstrated to exert athero-protective properties through the production of natural immunoglobulin M (IgM) class antibodies. Conversely, B cell depletion exacerbates atherosclerosis.
Vaccination

Despite all the primary and secondary prevention efforts and treatment, the incidence of ischemic cardiovascular diseases keeps growing to become one of the most common causes of morbidity and mortality globally. In response to this problem, researchers are attempting to identify alternative measures, with vaccination being one among them. Since atherosclerosis is an inflammatory disease where the immune system plays an active role in its initiation and progression, it would be desirable to look at strategies aiming at immune or inflammatory elements as a new method against atherosclerosis. One particular approach focusing on the immune elements is immune-modulation of the atherogenic adaptive immune response. An effective immuno-modulatory therapeutic approach must possess at least one of the following aspects:
- Arrests the development of the atherosclerotic plaque.
- Complete or partial regression of the plaque.
- Stabilizes the plaque.
- Reduces the inflammatory process involved in atherosclerotic plaque development.
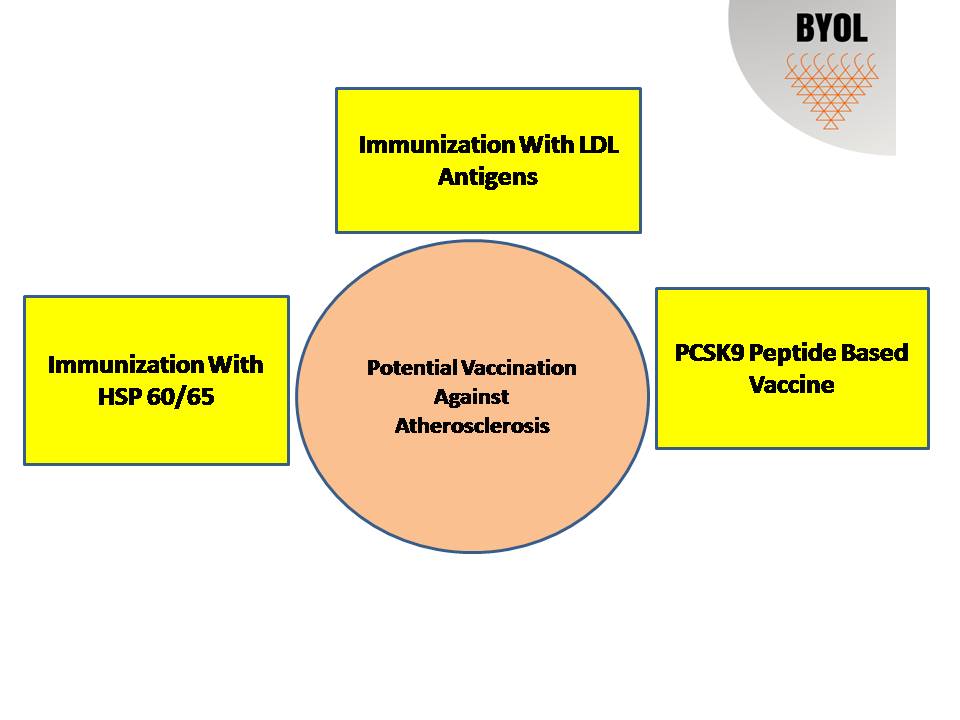
Several approaches have been investigated to look at the possibility of hindering atherosclerosis through active immunization or simply by the administration of antibodies against disease-related proteins involved in its development. Regarding vaccination against atherosclerosis, two aspects are crucial:
- Selective suppression of pro-atherogenic immune responses.
- Selective activation of anti-atherogenic immune responses.
Adjuvants
Adjuvants are substances that are mixed with vaccines to enhance the immunogenicity of highly purified antigens having poor immune-stimulatory properties. Adjuvants stimulate immune responses by one or more of the following mechanisms:
- Long-term release of the antigen at the injection site.
- Cytokine and chemokine upregulation.
- Cellular recruitment at the injection site.
- Increase in antigen uptake and presentation to APCs.
- Activation and maturation of APCs.
The most commonly used adjuvants are Freund’s adjuvant, which contains mineral oil and heat-killed mycobacteria and large quantities of HSPs, inducing adaptive immunity, and aluminum salt adjuvant, which primarily acts through preservation of antigens on the site of injection. Adjuvants inducing a shift to an anti-inflammatory Th2 response, e.g., aluminum and Freund’s incomplete adjuvant (which is mycobacterium-free), could be preferable as compared to adjuvants inducing Th1 responses.
Antigens
The most challenging step of immunization against atherosclerosis has always remained the identification of suitable antigens to induce sufficient protection against atherosclerosis. Antigens have been classified as:
Lipid Antigens
Lipid antigens mainly target the modulation of immune response against oxidized lipids or lipoproteins, which are key participants in atherogenesis.
Oxidized LDL (oxLDL)
- Mechanism: oxLDL is engulfed by macrophages, resulting in foam cells, a characteristic feature of initial atherosclerosis.
- Vaccination strategy: Induction of antibodies against oxLDL inhibits its uptake and foam cell formation.
- Example: Immunization with malondialdehyde-modified LDL (MDA-LDL) has shown protective effects in mice.
Apolipoprotein B-100 (ApoB-100) peptides
- ApoB is the protein moiety of LDL. Certain peptides from ApoB-100 have been employed to induce T-regulatory (Treg) reactions.
- Examples: p210 and p265 peptides have been found to inhibit atherosclerosis in murine models. These peptides facilitate the shift of immune responses from pro-inflammatory Th1 to anti-inflammatory Treg.
- Phospholipid antigens
- Oxidized phospholipids or lysophosphatidylcholine have been found to act as antigens.
Non-Lipid Antigens
These are proteins, peptides, or even whole pathogens that modulate atherosclerosis indirectly by changing the immune system or by acting on systemic inflammation.
Heat shock proteins (HSPs)
- Immunization with HSP peptides can trigger regulatory immune responses that restrain plaque formation.
- Studies have revealed upregulation of HSP60/65 in stressed endothelial cells.
β2-Glycoprotein I
- It is a plasma protein that is bound to negatively charged phospholipids.
- Immunization with β2-GPI or its domains has been shown to be protective in animal models, potentially by diminishing autoantibody production or inflammation.
PCSK9
- It is a protein that induces LDL receptor degradation, thereby increasing plasma LDL.
- PCSK9 vaccines elicit antibodies that neutralize its activity, thus decreasing LDL levels.
Pathogen-associated antigens
- Vaccines against cytomegalovirus or Chlamydia pneumoniae have been investigated in some studies because of their suspected association with atherosclerosis progression.
Oral DNA vaccination
The foundation of oral DNA vaccination is the target for certain cell surface proteins thought to play a role in atherosclerosis. With this approach, an expression plasmid that codes for the antigen delivers the genetic information from the carrier into host phagocytes in the gut. The phagocytes subsequently produce the antigen de novo in the cytosol and present it on MHC molecules.
Plant-based vaccination
- Plant-based vaccination as a possible tool for vaccination against atherosclerosis relies on the introduction of transgene into the plant cells using direct (introduction of DNA or RNA) or indirect (the use of plant bacteria and viruses) means.
- Plant-based vaccines compared to conventional vaccines, have easier storage, simpler route of administration, greater capacity to produce more intricate proteins with expected biological effects, are less expensive, and are better able to produce vaccines for a large-scale population.
Conclusion
The prevalence of atherosclerotic CVDs has prompted researchers to look into more efficient and long-lasting treatment methods. All the attempts of immunization against atherosclerosis have been aimed at strengthening athero-protective immunity and attenuating the pro-atherogenic immunity. Though highly commendable attempts have been exerted in this field, vaccination against atherosclerosis has not yet found a role in the prevention or treatment of atherosclerosis. There is a need to carry out studies to assess the efficacy of vaccination against the development of atherosclerotic plaques at the earliest stages. There is a long way to reach the ideal vaccination strategy, which could be utilized from early years of life to protect humans against atherosclerosis. It will not be achieved unless the investigators make inexhaustible attempts and funding organizations, governments, and universities provide financial support to research.
References
- M. Naghavi, A.A. Abajobir, C. Abbafati, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016 Lancet (2017), 10.1016/S0140-6736(17)32152-9
- T. Kimura, K. Tse, A. Sette, K. Vaccination to modulate atherosclerosis Autoimmunity (2015), 10.3109/08916934.2014.1003641
- M. Le Borgne, G. Caligiuri, A. NicolettiOnce Upon a Time: The Adaptive Immune Response in Atherosclerosis—a Fairy Tale No More. Mol Med (2015), 10.2119/molmed.2015.00027
- D. Mozaffarian, E.J. Benjamin, A.S. Go, et al. Executive summary: Heart disease and stroke statistics-2016 update: A Report from the American Heart Association Circulation (2016), 10.1161/CIR.0000000000000366
- Y. Pan, Y. Zhou, H. Wu, et al. A Therapeutic Peptide Vaccine Against PCSK9 Sci Rep (2017), 10.1038/s41598-017-13069-w
- C. Vlachopoulos, I. Koutagiar, D. Terentes-Printzios, et al. Relationship of PCSK9 levels with indices of vascular function and subclinical atherosclerosis in patients with familial dyslipidemias Hellenic J Cardiol, 60 (2018), pp. 124-128, 10.1016/j.hjc.2018.05.003
- E. Laere, A.P.K. Ling, Y.P. Wong, R.Y. Koh, M.A. Mohd Lila, S. Hussein Plant-based vaccines: Production and challenges J Bot (2016), 10.1155/2016/4928637