Pancreatic cancer is one of the deadliest and most difficult cancers to treat, with many patients being diagnosed when the disease is already advanced, in part because early symptoms are subtle.
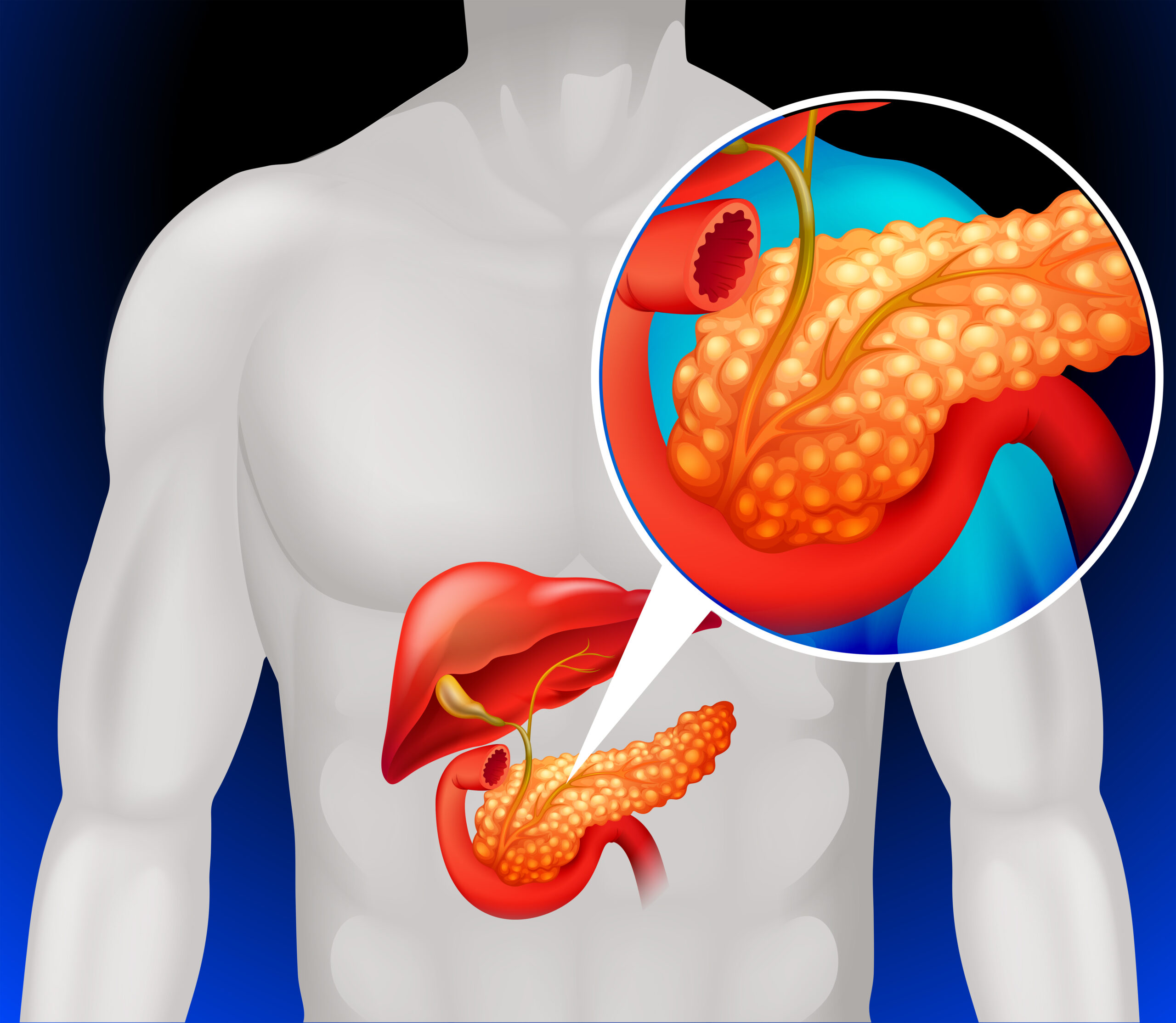
The pancreas, a large organ that lies behind the stomach, is important for digestive and blood sugar regulation. The key to combating the disease lies in understanding its risk factors, symptoms, and advancements in its treatment which can help disease detection early on and improve survival rates.
What is Pancreatic Cancer?
Pancreatic cancer starts in the tissues of the pancreas and falls into two general categories:
- Exocrine tumors (Pancreatic Adenocarcinoma) : Which account for approximately 90% of cases and originate in the cells that produce digestive enzymes.
- Neuroendocrine tumors (Pancreatic NETs) : These are less common and develop from hormone secreting cells. Generally, they have a better prognosis than exocrine tumors.
Causes and Risk Factors
The exact cause of pancreatic cancer is unknown, though there are some risk factors that increase its consistency:
● Smoking and Tobacco Use : Smoking is among the top modifiable risk factors for pancreatic cancer. For example, the carcinogens in tobacco can cause mutations in the pancreatic cells, triggering the formation of a tumor. Smokers are twice as likely to have pancreatic cancer than non-smokers.
● Family History and Genetics: Those who have a family history of
pancreatic cancer are at greater risk, particularly if there are mutations present in genes such as BRCA1, BRCA2 and PALB2. Genetic conditions like Lynch syndrome and familial adenomatous polyposis (FAP) also increase the risk.
● Chronic Pancreatitis : Chronic inflammation of the pancreas, which can occur from long-term heavy alcohol consumption or from having gallstones, can destroy pancreatic cells over time, leaving them vulnerable to cancerous changes.
● Diabetes and Obesity :
Individuals with type 2 diabetes, especially those with rapid-onset diabetes after the age of 50, have an increased risk of developing pancreatic cancer. Obesity is also involved, with excess body fat creating an insensitivity to insulin and an inflammatory milieu in the pancreas.
● Diet and Lifestyle Factors Trans fats, excessive alcohol, and a lack of physical activity also increase your risk of pancreas cancer. Red and processed meat rich diets have been associated with an increased risk, while fruits, vegetables, and whole grains may have protective effects.
Pathogenesis of Pancreatic Cancer:
Pancreatic cancer undergoes a multi-step process that starts with genetic mutations and advances to vigorous tumor growth:
Initiation: Mutations in the DNA of pancreatic ductal cells lead to loss of normal cell cycle regulation and uncontrolled growth.
Progression: The mutated cells escape immune surveillance, and acquire the ability to invade the surrounding tissues.
Metastasis: The cancer spreads via the lymphatic system and blood to other organs, including the liver, lungs, and peritoneal cavity.
Common molecular alterations in pancreatic cancer are mutations in:
● KRAS gene (in 90% of cases), which promotes uncontrolled cell division.
● TP53 gene, which protects against tumors but is commonly inactivated in cancer.
● SMAD4 is commonly mutated in more aggressive pancreatic cancer because it plays an important role in certain cell signaling pathways.
Symptoms of Pancreatic Cancer
Pancreatic cancer has been labeled a “silent killer” because the early signs are so subtle or absent. As the tumor becomes larger, symptoms may include:
Jaundice: Skin and eyes become yellow from yellowish bile accumulating behind a blockage of the bile duct.
Unexplained Weight Loss: A frequent early indicator, caused by poor digestion and appetite loss.
Abdominal and Back Pain: As tumors grow, they can put pressure on nearby organs and nerves.
Dark Urine and Pale Stools: Due to bile blockage.
Diabetes of New-Onset: Blood sugars elevate without previous patterns.
When these signs emerge, particularly in those who have risk factors, urgent medical assessment is essential.
Diagnosis and Staging
As early pancreatic cancer is hard to detect, a number of diagnostic approaches using:
Imaging Tests: CT, MRI, and endoscopic ultrasound (EUS) visualize tumors.
Blood tests: Tumor markers (e.g. CA 19-9) may be raised but are not reliable.
Biopsy: A sample of pancreatic tissue is examined for cancerous cells. Pancreatic cancer is staged similar to other cancers, from Stage I (localized) to Stage IV (metastatic) based on spread and tumor size.
Treatment Options
Treatment is determined by the stage of pancreatic cancer and the individual’s overall health. Surgery The only chance for a cure is the surgical removal of the tumors, which is only possible for 20% of patients at the time of diagnosis due to late-stage identification.
Whipple Procedure (Pancreaticoduodenectomy): The tumor and parts of the pancreas, bile duct, and small intestine are removed.
Distal Pancreatectomy: Removes the tail and body of the pancreas.
Chemotherapy: Given before and after surgery to shrink tumors and kill cancer cells.
● FOLFIRINOX (Combination therapy)
● Gemcitabine and Nab-paclitaxel (Combination therapy)
Radiation Therapy: Aids in shrinking tumors before surgery or relieving pain in more advanced cases. Often in combination with chemotherapy (chemoradiation).
Targeted Therapy and Immunotherapy
● PARP Inhibitors (Olaparib): Beneficial in selective instances, particularly with BRCA mutations.
● (Pembrolizumab) Checkpoint Inhibitors: A prospective option for a selected sub-group of patients whose genetic variations can be identified.
Prognosis and Survival Rates
Pancreatic cancer has a low survival rate from late diagnosis:
Localized stage: 5-year survival rate around 44%.
Regional spread: Survival drops to approximately 15%
Distant metastasis: Stage IV , Survival rate is under 3%.
Better survival outcomes result from early diagnosis, lifestyle changes, and clinical studies of new treatments.
Prevention Strategies
Although not all pancreatic cancer cases can be prevented, some steps can help lower risk:
● Stop smoking to reduce the likelihood of DNA mutations.
● Keep your weight in check to lower your risk of obesity.
● Eat lots of fruits and vegetables and whole grains.
● Avoid drinking alcohol.
● Screening for high-risk individuals (family history, BRCA mutations)
Conclusion
Pancreatic cancer poses a significant challenge due to its aggressive nature and late-stage diagnosis. Increasing awareness of risk factors and early symptoms, along with advances in treatment, can lead to earlier detection and improved outcomes. However, ongoing exploration of early diagnostic techniques and tailored healthcare also provide promise for enhanced survival rates going forward.
Reference
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17-48.
2. Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreatic cancers in the United States. Cancer Res. 2014;74(11):2913-21.
3. McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24(43):4846-61.
4. National Cancer Institute. Pancreatic Cancer Treatment (PDQ®)–Patient Version.