“Science is fun. Science is curiosity. We all have natural curiosity. Science is a process of investigating. It is posing questions and coming up with a method. It is delving in.”
Sally Ride
Novel cancer therapies such as immunotherapy have emerged over the past several years as there is a lot of heterogeneity in cancer and all the previously available therapeutic agents have fallen short of effective action against cancer. Immunotherapy is a paradigm shift in cancer treatment in the last 2 decades.
What is T-cell transfer therapy?
T-cell transfer therapy also known as adoptive cell therapy, adoptive immunotherapy, and immune cell therapy, is a type of immunotherapy, in which the might of your immune system is enlisted against the cancer. T-cell transfer therapies are of two types : Tumor-Infiltrating Lymphocytes (TIL) therapy and CAR T-cell therapy. They have some things in common, such as extracting T cells from the patient and growing them in the laboratory, and injecting them back into the patient intravenously through a needle.
How Does CAR T-Cell Therapy Work?
- T-Cell Collection: This therapy starts with T-cell collection from a patient’s blood by means of Leukapheresis.
- Genetic Engineering: Collected T-cells undergo laboratory modification to express CARs on their surface. CAR stands for Chimeric Antigenic Receptor. These CARs can recognize antigens found on the cancer cells. The process of growing T-cells in the lab may take between 2 and 8 weeks.
- Expansion: Expansion of these cells is achieved in a laboratory where CAR T-cells can proliferate into millions.
- Infusion: Once sufficient amounts of CAR T-cells have been generated, they are reintroduced into the patient’s bloodstream.
- Targeted Attack: These CAR T-cells will go on to circulate throughout the body, looking for and destroying cancer cells that produce target antigens.
TIL Therapy and CAR T-cell therapy: the similarities and the differences
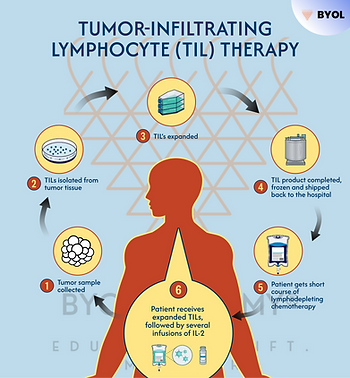
- TIL therapy uses tumor-infiltrating lymphocytes found in the tumor. These lymphocytes are tested in the lab to check their specificity for the tumor of interest. After determining which ones are the most reactive towards the tumor, the selected lymphocytes are treated with substances to enhance their growth in large numbers. The idea here is that the lymphocytes already present in the tumor or close to the tumor have previously shown a particular capacity to target those tumor cells. However, such lymphocytes may not be enough to destroy the tumor or to inhibit the signals that tumor are producing for the suppression of the immune system. By infusion of high amounts of these lymphocytes best in reaction with the tumor, it will help to overcome these barriers.
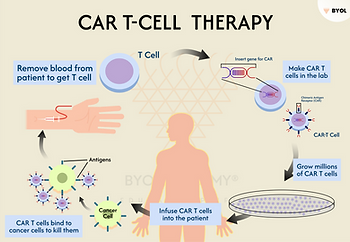
- CAR T-cell therapy is like TIL therapy, with a big difference that your T cells are changed in the lab to be able to produce a protein referred to as CAR before they are infused into you. CARs enable the T cells to adhere to certain proteins on the surface of cancer cells, thereby augmenting their ability to attack the cancer cells. This Therapy has worked well with blood malignancies and has successfully treated some patients with little or no chance of benefitting from standard treatments. Studies have revealed that 92% of patients with end-stage acute lymphocytic leukemia go to complete remission in clinical trials. However, the application of CAR T-cell therapy to solid tumors has been hampered by therapeutic obstacles including CAR T-cell expansion, persistence, trafficking, and tumor microenvironment.
Most cytotoxic approaches to neoplastic diseases remain poorly effective against advanced-stage disease. Another major challenge is the poor prognosis relapse rate because the response to therapy is different for each patient. Immunotherapy is one of the most exciting approaches in fighting many serious diseases, including cancers, autoimmune diseases, and hypersensitivity reactions because it exploits and enhances our innate immune systems. The basic concept of immunotherapy is that we harness the body’s immune response to destroy the cancer cells. This therapy relies heavily on the knowledge we already have about tumor progression, including the proximity of tumor cells to the immune system.
Types of cancers treated with T-cell transfer therapy
Lifileucel (Amtagvi), a T-cell transfer therapy, has been approved by the Food and Drug Administration (FDA) to treat melanoma and has also resulted in promising developments in Cervical Squamous Cell Carcinoma and Cholangiocarcinoma. However, the treatment remains experimental for these cancers. Currently, CAR T-cell therapy is primarily used to treat certain types of blood cancers, including:
· B-cell Acute Lymphoblastic Leukemia (ALL)
· Diffuse Large B-Cell Lymphoma (DLBCL)
· Multiple Myeloma
· Follicular Lymphoma
CAR T-cell therapy, a novel treatment technique, is an ongoing research area to develop its application in additional cancer types such as breast, lung, and pancreatic solid tumors.
Benefits of CAR T-Cell Therapy
- Targeted Treatment: In contrast to the conventional chemotherapy, which leads to a disturbance in all the healthy and cancerous cells, the CAR T-cell therapy is absolutely precise, aiming at the cancer cells only.
- Durable Responses: In several instances, cancer patients could stream through with long-term reliefs as brought about by the CAR T-cell therapy even in those cases when they were either at such very late stages or in those cases when the treatments have failed to mitigate the situation.
- Personalized Medicine: CAR T-cell therapy is a cellular treatment that is initiated by the patient’s own cells. It tends to be built on the genetic makeup and the cancer profile that is unique to each individual.
- Hope for Refractory Cancers: Among patients who show insufficient response to previous treatments, CAR T-cell therapy was anticipated to be the last option in the current case. It has been tried several times in patients and has succeeded in most cases, where patients have shown clear lesions following treatments other than CAR T-cell therapy.
Challenges and Risks
Although T-cell therapy is indeed a groundbreaking treatment, the fact that it has its downside must not be overlooked. T-cell transfer therapy does have side effects which may vary depending on the health status of the subject, type of cancer, tumor aggressiveness, choice of T-cell transfer therapy, and administered dose.
1.Cytokine Release Syndrome: It is a life-threatening complication caused by CAR T-cell therapy. It occurs because the T cells infused or other responsive immune cells that react with the new T cells release massive amounts of cytokines into the bloodstream. An instant increase in cytokines leads to complications such as:
- Fever
- Nausea
- Headache
- Rashes
- Rapid heartbeat
- Low blood pressure
- Difficult breathing
Most people have a mild form of Cytokine Release Syndrome, while in others, it can be severe or even life-threatening. CAR-T cells are meant to target proteins that are only found on cancer cells, though sometimes they target normal cells, thus producing a wide range of side effects such as organ damage.
2.Capillary Leak Syndrome: The sickness may be caused by TIL therapy and results from the leakage of fluids and proteins outside the small blood vessels into the neighboring tissues, leading to reduced blood pressure. Capillary Leak Syndrome may lead to heart failure, resulting in damage to other organs and the risk of shock.
3.Neurological Toxicity: Some patients among may show neurological side effects like confusion, seizures, or defective speaking. These symptoms are usually short-lived but still need a lot of close follow-up.
4.Cost: CAR T-cell therapy is very costly at the moment, with charges mostly going to hundreds of thousands of dollars. This expensive nature of the treatment may make it impossible for a lot of patients.
5.Limited Availability: Presently, only certain centers are CAR T-cell therapy providers, and this service is also not offered to all patients.
The Future of CAR T-Cell Therapy
The promising future of CAR T-cell therapy is beyond doubt. The developers are making an extra effort to conquer the current restrictions and extend the whole scope of this type of treatment. The primary focus areas are the following:
- Expanding to Solid Tumors: Despite the striking progress CAR T-cell therapy is seen to have in blood cancers, it is yet a big challenge to apply it to solid tumors. The researchers are working out how the removal of cancer cells can be used to destroy solid tumors to the last one.
- Reducing Side Effects: There are ongoing trials to generate new CAR T-cells with a safety level that is higher than that of traditional ones, i.e., the cells that do not induce side effects.
- Off-The-Shelf CAR T-Cells: Today, CAR T-cell therapy is a personalized treatment; it necessitates the utilization of the patient’s own cells. However, because patients are now treated with their own cells, researchers are also trying to create “off-the-shelf” CAR T-cells that can be made in advance and used for many patients, possibly lowering costs and wait times.
- Combination therapies: Combining CAR-T cell therapy with other treatments such as checkpoint inhibitors or targeted therapies may improve the efficacy of CAR-T and lead to improved patient outcomes.
Conclusion
- CAR T-cell therapy is a huge step in the battle against cancer. It uses the immune system to transform and rejuvenate the lives of many patients with virtually no other options. Despite the challenges, the speed of research and development in this area indicates that we are only at the beginning of CAR T-cell therapy, and we can expect even more benefits in the years to come.
- For patients and their families, CAR T-cell therapy is more than a treatment. It is a testament to the amazing potential of science and medicine to change lives. CAR T-cell therapy, an innovative and life-changing approach, is a beacon of hope leading to a future where cancer can be transformed from a fatal diagnosis to a manageable condition.
Call to Action
For anyone who may be considering CAR T-cell therapy for themselves or a loved one, it’s important to discuss this treatment option with your healthcare provider to see if it’s right for you. So keep yourself informed, reach out with questions and explore all the resources on hand to guide you towards the best choice for you and your health. Let’s continue working together in pushing the boundaries of possibilities of conquest in the battle against cancer.
References
1. Miliotou, A.N. and Papadopoulou, L.C., 2018. CAR T-cell therapy: a new era in cancer immunotherapy. Current pharmaceutical biotechnology, 19(1), pp.5-18.